The babies are doing just fine
A landmark study dramatically improved the survival rate of very preterm babies. Half a century on, the Auckland Steroid Study continues to deliver good news

It was January 1974, and for Susan Wright it was just an ordinary day. Until it wasn’t. Susan, who was pregnant, wasn’t feeling great as she headed off on the bus to work as usual, from the small Auckland flat she shared with husband Charlie.
When she felt worse later in the day her boss told her to head home, but it was only when the bleeding began she realised with horror she was going into labour – at just 27 weeks.
In 1974, the prognosis for babies born between 24 and 28 weeks wasn’t good at all; only about one in five survived. And one of the biggest problems was that the lungs of these tiny babies just weren’t developed enough to breathe outside the womb.
Not that Susan knew that at the time.
She headed straight to National Women’s Hospital, where doctors hooked her up to a variety of machines and administered drugs designed to slow down or halt labour.
They also offered her something else – something new and experimental in the obstetrics world at that time – two painful injections in her buttocks of a steroid study medication.

NEW DAD: Charlie Wright cradles baby Amanda.
NEW DAD: Charlie Wright cradles baby Amanda.
NEW MUM: Susan Wright and Amanda.
NEW MUM: Susan Wright and Amanda.
When Susan went into labour that January day, she opted to become part of the Auckland Steroid Study – a first-in-the-world randomised controlled trial of antenatal steroids being carried out at National Women’s. Between 1969 and 1974, 1,200 women at risk of giving birth early received either corticosteroids, or a matching placebo, before the baby was born.
Researchers believed steroids given to mothers could give a boost to a premature baby’s lungs – enough to give the newborn a fighting chance. The study wanted to find out whether the babies whose mums got the steroids had better survival rates and health outcomes versus the ones whose mums got the placebo. They also wanted to find out if giving steroids to mums was safe for them and their babies.
Neither Susan nor her doctors knew at the time if she was getting a steroid or a placebo, but it turned out Susan was one of the steroid mums. After four traumatic, confusing days in suspended labour, and those two steroid injections, Susan Wright gave birth to her first baby. Amanda was 28 weeks gestation, weighed just 1.3 kilograms – about the same as a biggish pineapple – and needed ten weeks in the neonatal ward before Susan could take her home.
Amanda Wright was one of those Auckland steroid babies – her arrival and survival from a rocky start almost certainly improved by the treatment that has now become widely adopted, savings hundreds of thousands of babies born too early.
(See sidebar: Saving the babies born too early)
Amanda was always very short for her age, found it difficult to feed as a baby, and almost died of pneumonia when she was six months old. Fifty years on, Susan and ‘baby’ Amanda sit on the sofa in Susan’s Oratia, Auckland home and reminisce. There are photos of a tiny baby in an incubator, and of that same baby’s recent 50th birthday, surrounded by friends and family.
Susan remembers that Amanda as a child was always small, determined, happiest buck naked in a pair of red gumboots, stomping around their section. She also remembers coming in sometimes during the traumatic early weeks when Amanda was in an incubator and seeing crying families and a priest delivering last rites.
Mother and daughter know how easily that could have been their family. “I don’t think I’d be alive if it wasn’t for the steroid treatment,” Amanda says. “My parents, my grandparents always told me I was a ‘special baby’.”
Susan, Amanda and all the other mums and babies who’d taken part in the Auckland Steroid Study didn’t know it, but doctors still worried about the impact of steroids on those babies as they grew up.

“It was clear there were short-term benefits, but steroids are potent medications, and some have serious side effects,” says Anthony Walters, a doctor at the Green Lane Clinical Centre, Auckland and a PhD researcher at the University of Auckland’s Liggins Institute.
“There have been concerns that giving them to pregnant women, whose babies are still developing, could affect the health of these babies later in life, even into adulthood.”
Walters’ research, just published in the respected journal PLOS Medicine follows up the now 50-year-old children of the study mothers in the Auckland Steroid Study to see if the steroids have had any long-term impacts on their health, particularly in terms of heart disease and related conditions.
Walters found no adverse consequences. “We’ve proven we don’t need to worry. We are confident that although preterm babies have a whole range of health problems as they grow up, these are not caused by the steroid.”
It’s good news for Amanda and her study peers. But it’s also good news for researchers looking at how steroids might be used as treatment with other babies – for example, ones where the mum goes into labour after 34 weeks, or ones where the baby is due to be born by caesarean.
“There are ongoing trials in these areas,” says Professor Dame Jane Harding of the Liggins Institute fetal and neonatal research team. “This study provides reassurance these trials should go ahead.”
Amanda says being part of the follow up research programme called ANCHOR has been “fascinating”. She feels some pride in how a half century later the processes and doses used in the Auckland Steroid Study are still used, not just in New Zealand but all over the world. She says. “To be honest, it’s a pretty special thing to have been involved in.”
“We’ve proven we don’t need to worry. We are confident that although preterm babies have a whole range of health problems as they grow up, these are not caused by the steroid.”
"To be honest, it's a pretty special thing to have been involved in."

Saving the babies born too early
The history of the research that became the Auckland Steroid Trial is an extraordinary story of genius, perseverance – and a touch of luck. And it started with one Auckland obstetrician and researcher, Graham (later Sir Graham) Liggins – known to everyone as Mont, after a childhood obsession with Monty the Mouse. Mont became fascinated with the process of labour and birth, particularly the mechanisms that cause a pregnant woman to go into labour. He became convinced it was the fetus, not the mother, who was responsible for the timing of labour.
Using sheep he kept in a field in Cornwall Park, just behind the hospital, and transported in his own car to a makeshift laboratory set up in an abandoned shed, Mont Liggins started giving steroids to pregnant ewes to accelerate birth and study the mechanisms of labour.
And then something extraordinary – and unexpected – happened. Mont noticed that many lambs that were born prematurely and whose lungs should not have been mature enough to allow them to breathe normally, were surviving. Sir Peter Gluckman was the first director of the institute named after Mont Liggins, and a mentee and colleague. He told the story of what happened next in an eulogy he wrote after Professor Sir Graham 'Mont' Liggins death in 2010.
“This was an accidental finding but one of enormous importance – a very rare moment in science, one most scientists would have missed … At that time, to be born two to three months premature was often a death sentence – the lungs could not work, they were too immature to stay distended and the air sacs were not properly developed.
“What Mont had discovered, and what he quickly turned his immense talents to, was that steroid hormones could accelerate the maturation of the lungs. So, if he gave the fetus the hormone cortisol before the age at which the fetus would normally have made it, the lungs matured, the baby could be born prematurely, and its lungs would work well enough for survival to become possible.
“And he realised he could give a form of the hormone to the mother, and it would cross to the fetus and also work.”
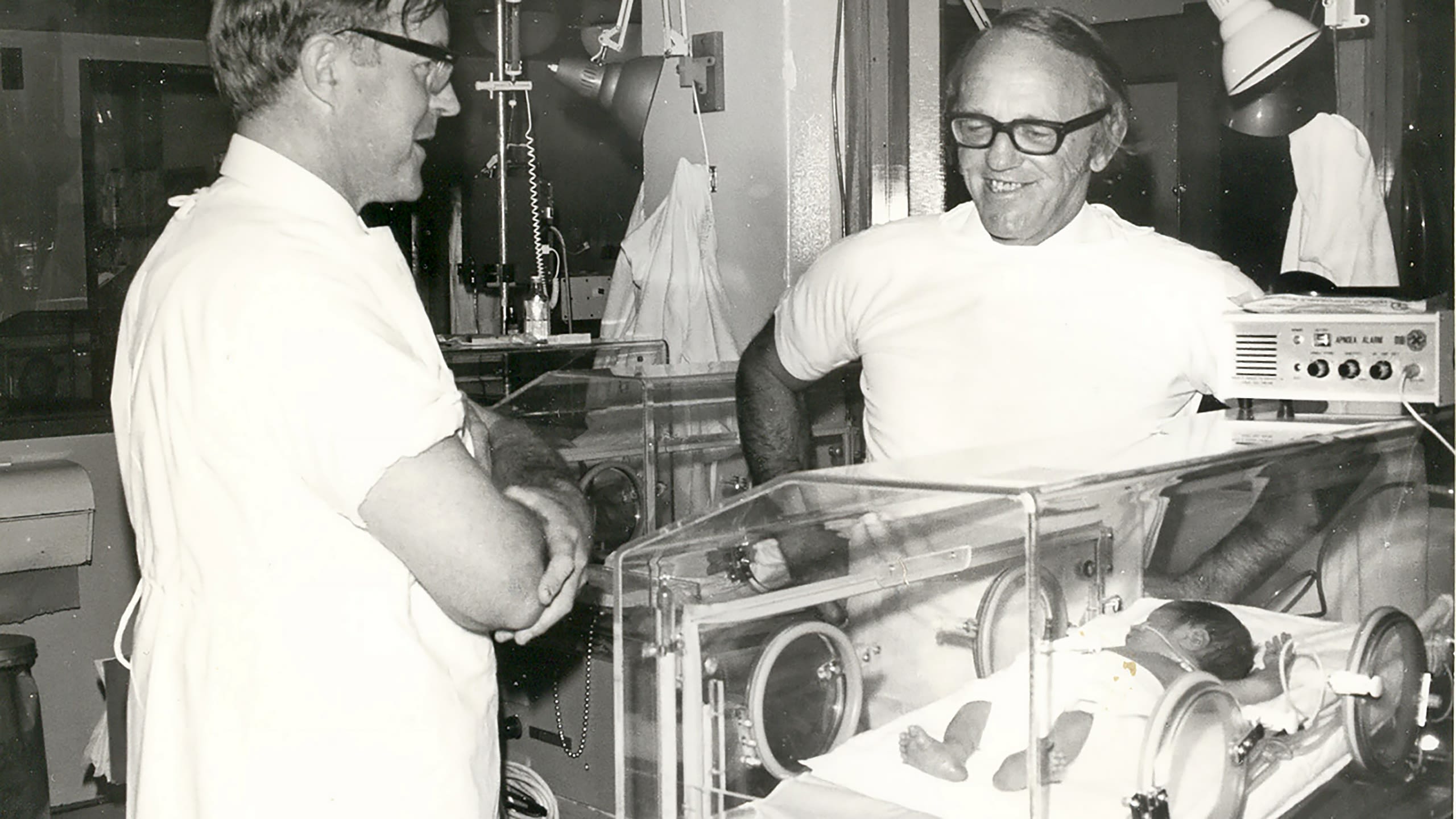
With a speed “that seems incredible by today’s standards”, Mont teamed up with Auckland paediatrician Dr Ross Howie and started a clinical trial giving steroid hormones to mothers in premature labour. And it worked.
The study proved premature babies whose mums were given the steroids were significantly less likely to die. Steroids changed the field, from most babies born before 34 weeks dying, to most surviving. Hundreds of thousands of tiny babies have been saved worldwide.



