New hope for children with cerebral palsy

Cutting-edge tools once reserved for astronauts and data scientists are now reshaping rehabilitation for children with cerebral palsy.
Auckland Bioengineering Institute researchers are blending physics, medicine and machine learning to understand how movement breaks down – and how to restore it.
Imagine a child who’s needed help to walk their whole life because their muscles can’t quite do what their brain tells them to.
Now, picture that child moving freely on a treadmill, lifting their arms in the air and laughing as they watch television.
It’s something being made possible by NASA-developed anti-gravity technology at the Auckland Bioengineering Institute (ABI), where researchers are confronting Aotearoa’s leading cause of childhood physical disability: cerebral palsy (CP).
Affecting an estimated one in 500 Kiwi kids, cerebral palsy stems from damage to the developing brain, which disrupts the signals that coordinate movement and posture.
That disruption can make even simple movements slow, stiff or unbalanced. But the ‘Alter-G’ anti-gravity system being tested by children as part of a project at the University of Auckland – Waipapa Taumata Rau’s Auckland Bioengineering Institute, is redefining what physical control feels like.

At the start of each session, the kids are fitted with a heart-rate sensor and treadmill shorts that enclose their lower body in a sealed air chamber. As the chamber inflates, they’re lifted from the waist, unloading up to 80 percent of their body weight.
Next, they’re encouraged to explore new movements and to walk on their own – all while ABI researchers monitor their heart rate to keep them in a safe, moderate effort range.
By lightening their load, ABI team leader Dr Pablo Ortega-Auriol explains, the children can be more selective in activating the muscles that drive walking.
This helps retrain both muscles and neural circuits, leading to lasting improvements in gait and movement quality.”
The approach is delivering clear results – even once they emerge from their anti-gravity environment. Some children are walking up to 40 percent faster and farther, and families say they’re more active and confident beyond the sessions.
Yet even with those gains, the lab still feels more like play than therapy.
“We watch anime, listen to music, sing if they want to,” Ortega-Auriol says. “We build a good relationship so that exercise feels positive – something they enjoy rather than a task.”
Seeing the grins on their faces as they realise what their bodies can do is a reminder of why he’s dedicated much of his career to tackling cerebral palsy, he says. “A lot of people might struggle with the purpose of the work, but I don’t, as I get to see those smiles.
“It’s very rewarding.”

Every three days a baby is born with cerebral palsy in New Zealand
Cerebral Palsy (CP) – Hōkai Nukurangi is a physical disability that affects movement and posture.
It is an umbrella term that refers to a group of permanent and lifelong conditions caused by damage or disturbance to the brain during its development.
The way CP impacts a person’s movement and posture depends on when the brain damage occurred, and which parts of the brain are affected.
People living with CP can have difficulty with movements such as walking, keeping their balance and using their hands in everyday tasks. They may have other medical conditions, including epilepsy, and/or difficulties with seeing, learning, or talking.
The disturbance or damage to the development of the brain mainly occurs during pregnancy, birth or very soon after birth (for approximately 9 out of 10 people with CP).
Damage to the brain, resulting in a CP diagnosis, can also occur after one month of age, up to two years of age (for approximately 1 out of 10 people with CP).
There are many possible causes, risk factors and/or events that can lead to CP. Sometimes the exact cause leading to the damage is unknown.
For all types of CP, the initial damage to the brain often stays the same. The impact of CP and its features, like spasticity, can change over time as people grow up and as they age.
In New Zealand:
- Cerebral palsy is the most common physical childhood onset disability
- It occurs in approximately 1 in every 500-600 babies born
- A baby is born with cerebral palsy every 3 days
- It is estimated that there are up to 10,000 people living with it.
The Cerebral Palsy Society of New Zealand is a member-based charity that supports people who live with CP, and their whānau.

The simple truth driving research
The Auckland Bioengineering Institute's wider cerebral palsy research programme, which blends physics, physiology and anatomy through computational modelling, is built around a simple truth: understanding comes before intervention.
“Understanding the real mechanism of what’s going on is always critical to having the best approach for intervention and treatment,” says Professor Thor Besier, who leads the bioengineering institute’s Musculoskeletal Modelling Group.
Without that understanding, you’re always going to be limited in how you can improve a child’s day-to-day life.”
If Ortega-Auriol’s work is about retraining movement, Dr Julie Choisne’s focus lies in understanding its underlying structure: how bones grow, deform and can be measured to guide more precise treatment.
Working with University of Auckland orthopaedic surgeon Professor Sue Stott, Choisne helped create a world-first growth atlas of the paediatric skeleton, drawing on a rare forensic dataset of CT scans from more than 300 children aged four to 18.
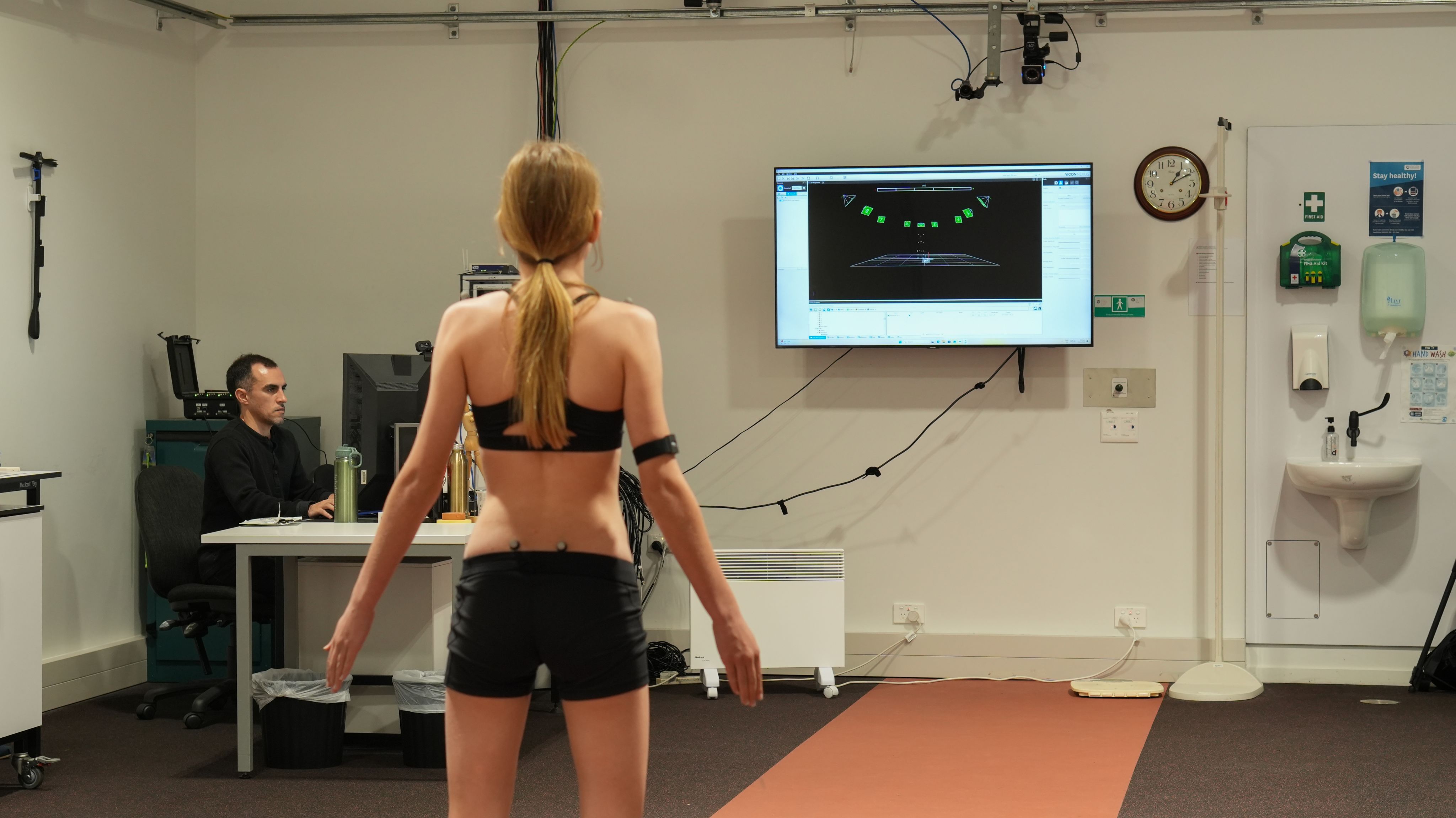
Now, Choisne’s team is translating that modelling into clinical tools that could make gait analysis far more accessible.
Her doctoral student Enzo Allevard is developing a low-cost system that combines 3D scanning with wearable motion sensors, allowing clinicians – and potentially even families – to analyse a child’s movement without specialised labs.
By predicting each child’s bone geometry and precisely locating the sensors, the system generates accurate musculoskeletal models to support clinical decisions such as surgical planning or brace design.
Faster and less data-intensive than conventional gait labs, it could also open access for whānau living in rural communities and provide new insights into muscle forces and joint loading.

AI trials to support early diagnosis
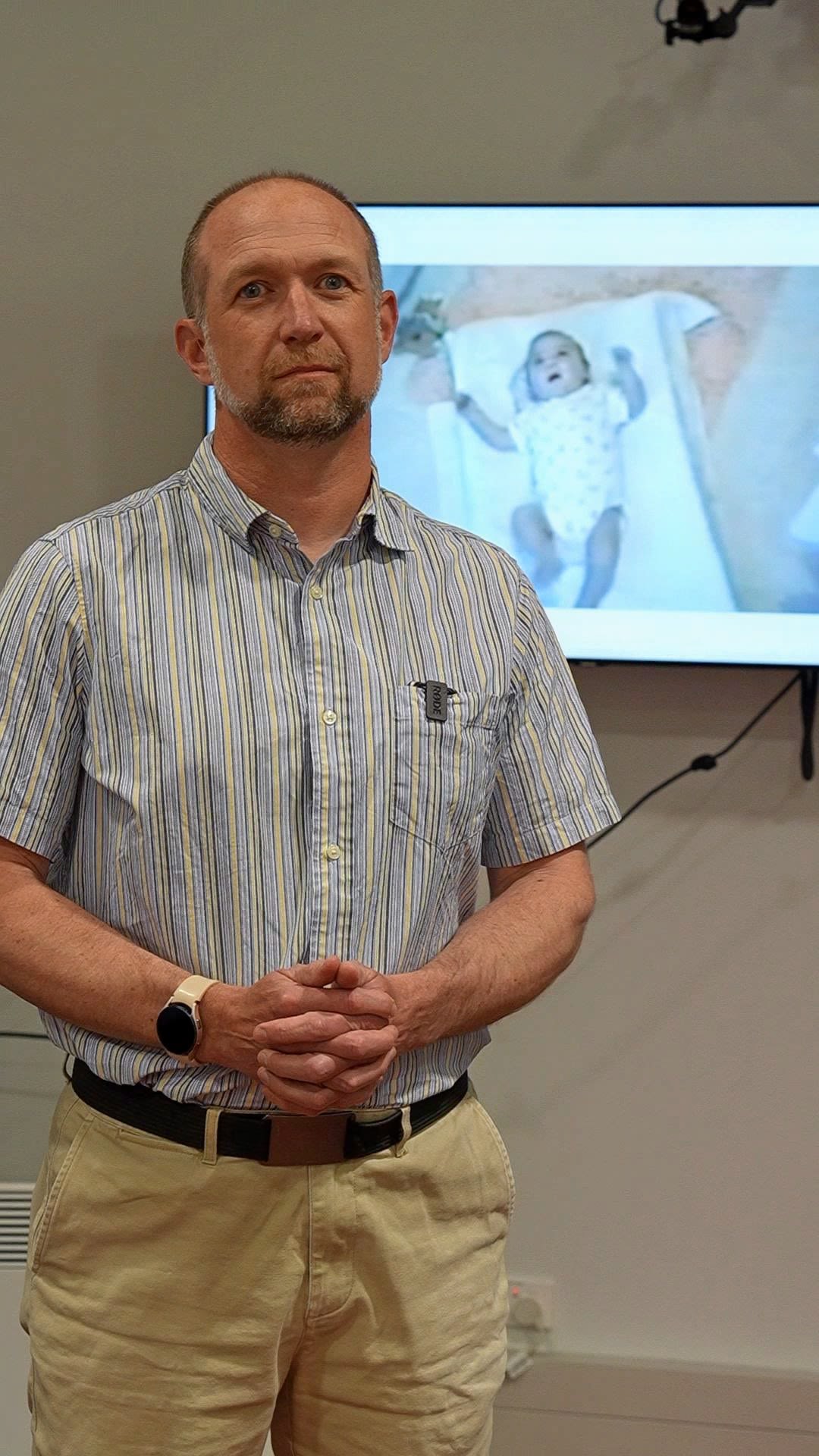
Another group, led by Dr Angus McMorland of the Department of Exercise Sciences, is taking the focus to the very beginning: finding ways to detect cerebral palsy within the first months of life.
His team is using artificial intelligence (AI) to automate the gold-standard General Movements Assessment (GMA) for infants’ neurological development, and later risk of CP.
McMorland explains the existing method relies on trained assessors to watch short videos of babies lying on their backs and categorise their spontaneous movements as normal, abnormal, or absent.
“With the AI technology, we can analyse exactly the same videos the clinicians are already collecting for the manual version of the assessment,” McMorland says.
The aim is to make early diagnosis faster, easier, and far more widely available: particularly for the 40 percent of children with CP who have no obvious risk factors and would otherwise be missed.
“For a system to be widely adopted into real clinical practice, it needs to add as little extra work for the clinicians as possible.”
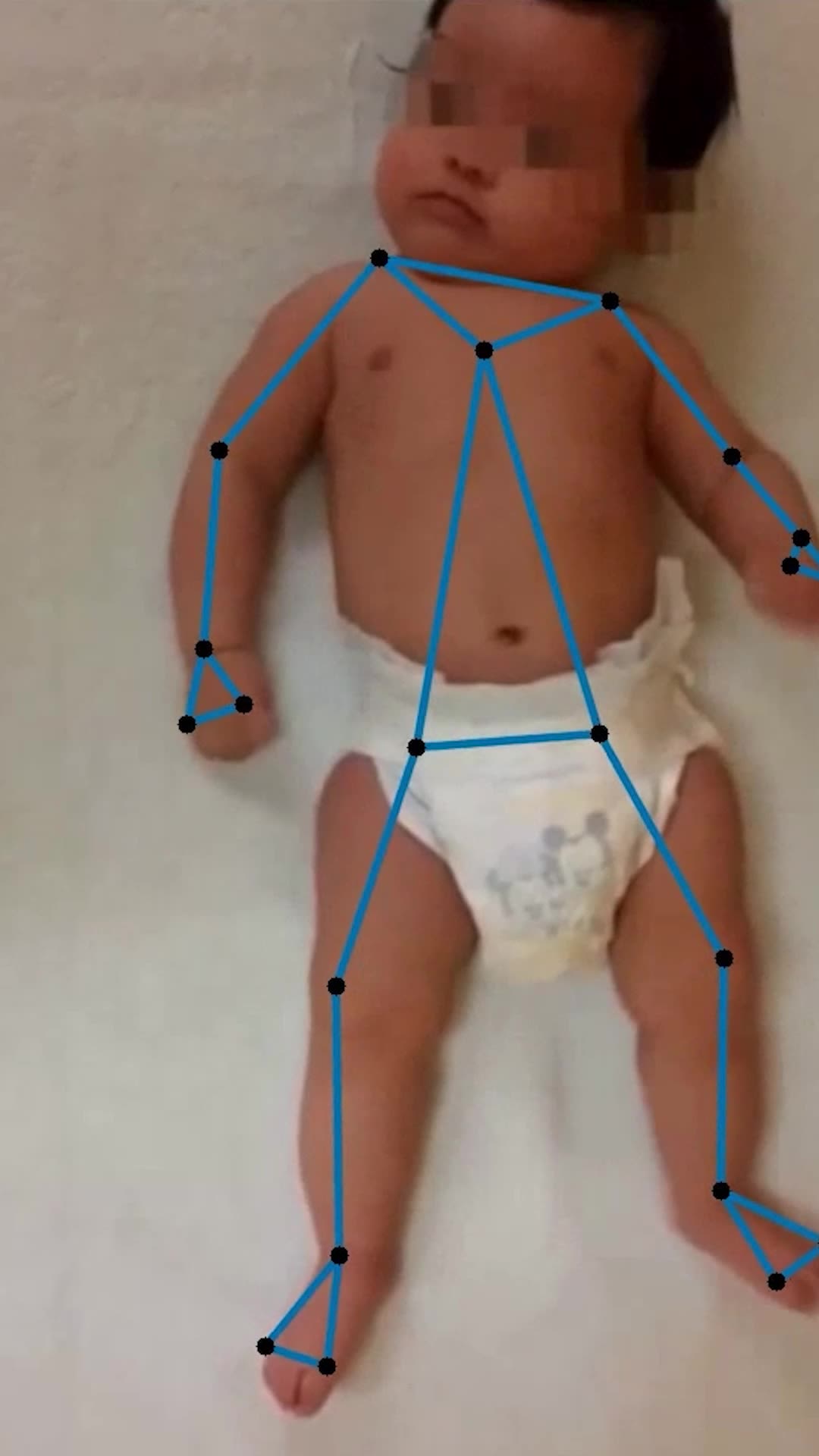
So far, his team has developed an app for clinicians to securely record and upload videos, a computer vision system to track babies’ movements, and an AI classifier that can distinguish between normal and abnormal patterns.
“While there are a few other efforts around the world to do the same task, our computer vision system captures additional clinically relevant movement features that we think will increase the sensitivity of our approach.”
Early intervention, McMorland says, has the potential to change the course of a child’s life. “The development of our neurons, muscles and bones is all activity-dependent: their normal development relies on movement and sensory input from the environment, but they also enable that movement and sensory input,” he says.
“This creates a feedback loop that can turn into a vicious cycle when early injury to the brain disrupts the process.” Intervening within that loop, he explains, can have “disproportionately big effects.”
Overseas trials are beginning to show the benefits of breaking this cycle as early as possible in a child’s development, McMorland says – something that can’t happen without early diagnosis.
For example, a treatment approach for babies under a year old, known as GAME (goal–activity–motor enrichment), sees parents guiding their child through a programme of ‘self-generated movement’ – from tasks encouraging the babies to sit on their own, to ones pushing them to grab or hold different objects.
Results from the programme suggest gains in motor function, adaptability and independence for the babies, and a valuable sense of agency for parents.
Another treatment, CIMT (constraint-induced movement therapy), focuses on infants with one-sided impairments, gently restricting the stronger arm to encourage use of the weaker one.
CIMT has shown evidence of improved motor function in the affected limb, and again, parents report feeling empowered by their involvement.
“We’re pretty confident from our understanding of the basic physiology of developing nerves, muscles and bones that early intervention has to help,” McMorland says.
“One problem with tests up until now has been not being able to identify well the at-risk group of children who are the ones where we should test and fine-tune interventions.
“Our assessment method, by identifying at-risk infants at greater scale and more accurately, will help with this.”
McMorland hopes to see their AI-assisted early diagnosis tool eventually used routinely across New Zealand, including in rural settings where access to trained assessors is limited.
Down the line, I definitely can see this technology becoming a regular screening tool, as it would be easy for whānau to record the videos at home and send them to us for analysis.”
Research and impact founded on spirit of partnership
Now more than a decade in the making, the Auckland Bioengineering Institute's cerebral palsy research has always been a story of collaboration and curiosity.
What began from work between the ABI's international expert in musculoskeletal modelling Professor Thor Besier, paediatric orthopaedic surgeon Professor Sue Stott and others grew into a world-leading programme, with the arrival of Dr Julie Choisne , a specialist in human biomechanics with experience in France and the United States and Dr Geoffrey Handsfield a musculoskeletal bioengineer from the University of Virginia, adding further momentum. “Having them here gave the work real impetus,” Besier says.
Two major philanthropic gifts, granted to the ABI in 2022, have meanwhile helped the team push into new territory.
The Friedlander Foundation, established by Auckland philanthropist Sir Michael Friedlander, committed $2.95 million to a five-year project developing tools for early detection and treatment of neurological disorders in infants.
Their support stems from personal experience: Sir Michael's granddaughter Maia, born with cerebral palsy, was one of the first Australasian children to undergo a pioneering stem-cell transplant overseas.
The second gift came from Carlo and Julie Fiorentino, a married couple who both lived with cerebral palsy and left their estate to the ABI when Carlo died in 2021.
Their bequest created the Carlo and Julie Fiorentino PhD Scholarship in Movement Disorder, supporting research that reflects their lifelong belief in independence and opportunity for people with disabilities.
Besier says this spirit of partnership between engineers, clinicians and donors is what sets the ABI apart globally – along with its unique blend of data-driven tools and physics-based insight.
Artificial intelligence is invaluable, he says, for automating complex computational tasks such as segmenting medical images to build patient-specific models. But it can’t replace fundamental scientific understanding.
“For some applications, AI is tremendous,” he says. “But for other applications, you still need the laws of physics and physiology that govern an individual patient to really come up with a good outcome.”
He points to surgery as one example. Machine-learning systems are now being trained to predict which children with a “crouch” gait might benefit from muscle-tendon lengthening - a common but often blunt surgical procedure.
While AI can identify statistical patterns and forecast which children are likely to respond, it ignores the underlying muscle physiology and neurological control.
“Children who respond well might do so for very different reasons,” Besier says. “Without understanding those mechanics, we can’t refine or improve the treatment itself.”
And despite remarkable progress, Besier says some of the biggest questions about cerebral palsy remain unresolved.
One enduring challenge is understanding how early brain injury cascades into the complex muscle and bone deformities that emerge later in childhood.
Another is achieving reliable early diagnosis: identifying CP in infants as young as six months.
A third, and perhaps most critical, lies in determining which treatment approaches work best at different stages of development to harness the brain’s plasticity while it can still adapt. Ultimately, Besier says, the goal remains the same: to give every child the best possible chance at independent movement.
If we can understand how and why things go wrong, we can help make them go right – and that’s what drives all of us.”



