Blue skies thinking the foundation of innovation
The real story behind scientific 'breakthroughs' is basic research, hard slog and serendipity
By Nikki Mandow

Kitea Health’s 'breakthrough' in a US$2 billion market shows the unique role universities perform as engines of innovation by uniting blue sky thinking, researchers from many disciplines, and industry.


Kitea’s brain sensor relies on physiology, electronics, engineering and chemistry. Without deep expertise in each area, it would not exist
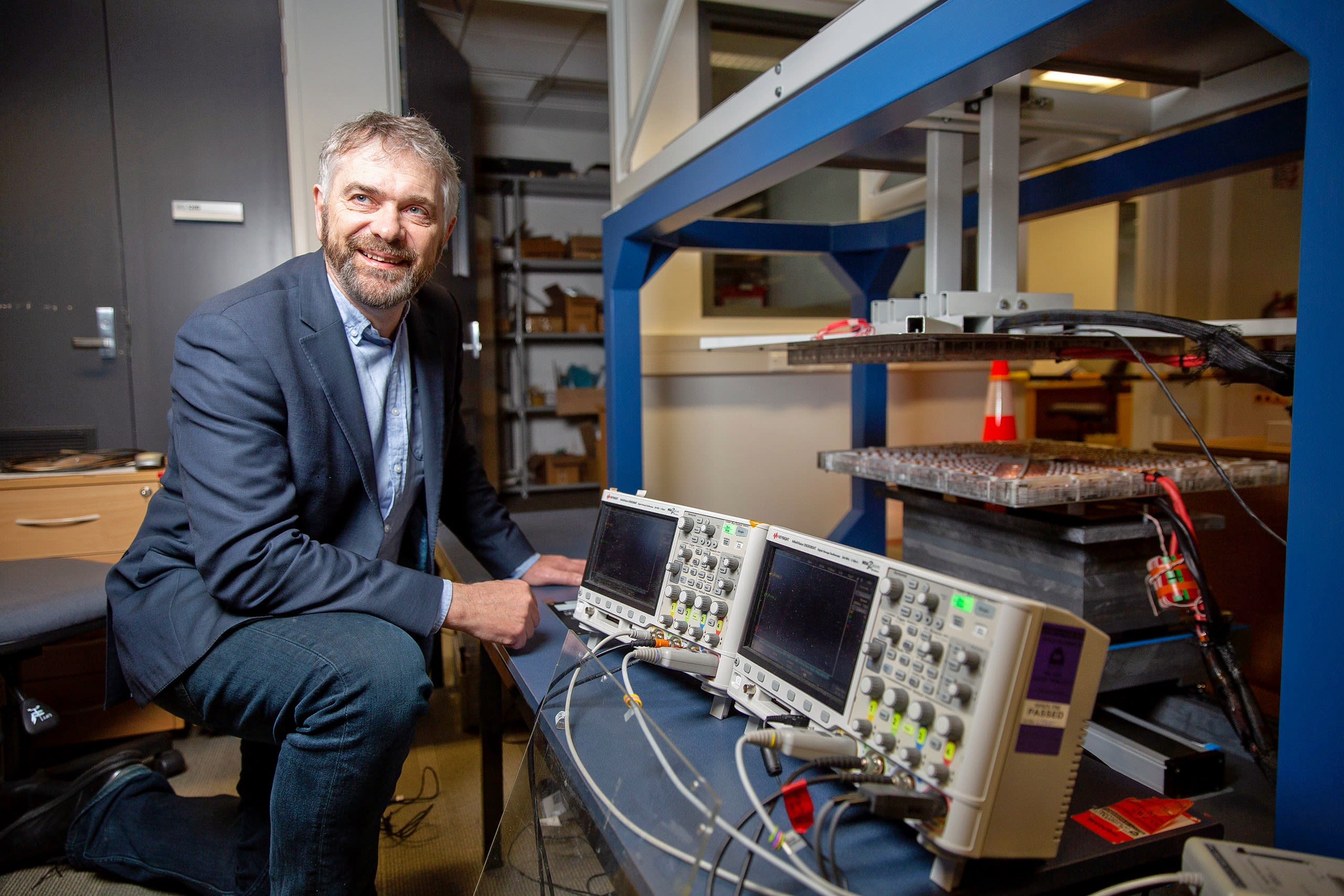
Professor Simon Malpas – in striped bow tie, peacock blue dinner jacket and sartorial specs – walked on stage at the TSB Arena in Wellington to receive the prize for ‘Most innovative deep tech solution’ at the 2025 New Zealand Hi-Tech Awards. As the audience applauded, most would have been unaware of the depth and breadth of the research behind the implantable brain sensor developed by Malpas’ company, University of Auckland spin-off Kitea Health.
Neither would they have suspected that the research came from a wide range of disciplines some seemingly distant from the final medtech product: engineers studying wireless power for heavy industrial applications, physiologists looking at the cardiovascular system of rats, chemistry professors trying to make big gadgets tiny.
But without them, as Malpas says: “None of this would have been possible”. Imagine the science community as a bunch of atoms in a coffee cup, Malpas says, "In the process of bouncing around with each other they talk and share ideas and so often that results in something dramatic. Think about Nobel Prize winners. Often quite disparate groups have come together through some process, shared ideas and realised they have something to contribute to each other.”
There is no reason why this shouldn’t happen in the private sector – and sometimes it does. But in a corporate setting, commercial pressures can get in the way of collaboration. “That’s the great thing about a university,” says Malpas, who remains a Professor at the Auckland Bioengineering Institute as well as chief executive of Kitea Health. “There’s a diversity of thought and expertise and people talk to each other.” International conferences and peer-reviewed academic papers create an environment where knowledge is shared locally and around the world, he says.
If you don’t have the life-threatening brain-swelling condition known as hydrocephalus, you have probably never heard of Kitea Health, nor its award-winning pressure sensor which can help patients and their families manage it. But for the 100 children diagnosed each year in New Zealand, or the estimated 15 million sufferers worldwide, it’s a medical breakthrough.
The sensor, about the size of a chunky half matchstick, is implanted into the brain and activated from outside the skull using a “wand” like a stubby table tennis bat with a hole in the middle. Its job is to allow patients and their families to see if fluid is building dangerously in their brain.
Kitea Health figures show annual healthcare costs associated with hydrocephalus sensing in the US alone are around $US2 billion. The global cardiac monitoring market, which Kitea plans to target in its next phase, is projected to grow from US$8 billion in 2022 to US$20 billion by 2032.
The words ‘medical breakthrough’ are like the term ‘overnight success’; they make the scientific innovation process sound quick and dramatic. Instead, breakthroughs are almost always the result of years of hard-slog scientific research, sometimes by multiple teams, combined with a bit of luck and the occasional random but serendipitous meeting.
Sir Alexander Fleming’s discovery of penicillin in 1928 was described by British haematologist and biographer Gwyn Macfarlane as, ‘a series of chance events of almost unbelievable improbability”.
The story of the then unknown scientist coming back from holiday to find mould had contaminated one of his petri dishes and killed the staphylococci bacteria that should have been growing is well-known.
Less revolutionary is the fact the petri dish discovery followed Fleming working for almost two decades on bacterial infections – his research history meant he understood what he was seeing.
Even then penicillin languished unappreciated for more than 10 years after Fleming discovered it; it took a different research team developing the idea further before it actually become available as a miracle drug - and won the three scientists a Nobel prize.
“A series of chance events of almost unbelievable improbability”.
The backstory of Fleming’s discovery rings true for Simon Malpas. In the 1990s, Malpas was a physiology professor looking at how different body systems worked in animals, as a way to understand how these same systems could go wrong and cause problems in humans.
The work involved measuring tiny electrical signals in the animals over many months, but there were problems. Wired gadgets restricted animals’ movement and made infections more likely, but batteries made implantable devices too big and clunky.
“One day I was in the tearoom on the 12th floor of the Engineering Building. I had gone to see someone about something else, but found myself having a conversation with an engineering professor called John Boys and I told him about our problem with these implanted devices for animal studies.”
Professor John Boys knew virtually nothing about implantable sensors; but he just so happened to be one of the leading experts in the world on wireless power. These days so-called ‘inductive power transfer’ is used for everything from charging mobile phones and smart watches to running heavy manufacturing lines and theme park rides.
But when Boys first started working in the field in the late 1980s it was firmly in holy grail territory. Boys’ work would indirectly lead to the establishment of spin-out wireless power development company PowerbyProxi, eventually sold to Apple for an undisclosed multi-million dollar sum.
Boys would also found, with Professor Grant Covic (still working in the field at the University of Auckland), global start-up company HaloIPT. HaloIPT focused on electric vehicle wireless charging infrastructure and was sold to Nasdaq-listed computer chip company Qualcomm in 2011 in what was claimed at the time to be the biggest commercial deal by a New Zealand university or Crown Research Institute.
Boys, now retired, and Covic would end up with more than 100 patents under their belts, in a range of different areas; their foundation work would also be useful in the development of the hydrocephalus brain sensor.
But as is typical with research, John Boys didn’t start his career in the field of wireless power. “It was serendipity,” Covic says. “John was working on DC to AC [direct current to alternating current] converters and his original goal didn’t work out. But it led him to think the technology could be used in wireless power. So along with [fellow University of Auckland professor] Andrew Green we started investigating that.”
High-precision medical technology was not even on the radar. But the collaboration on implantable monitors for Malpas’ rat experiments would be a critical early step for the development of the Kitea Health brain sensor. It would not be the only one.
Boys’ work would indirectly lead to spin-out wireless power company PowerbyProxi, eventually sold to Apple for an undisclosed multi-million dollar sum.
Wireless power and brain sensors
The whole idea for the brain pressure sensor was sparked by an email to the Auckland Bioengineering Institute team from Starship Childrens' Hospital’s Dr Peter Heppner. The paediatric neurosurgeon wanted to know if Malpas could help with a problem he and colleagues around the world had with the life-threatening brain condition hydrocephalus.
Hydrocephalus has been treated for decades by inserting a tiny silicon tube, which drains excess fluid from the brain harmlessly into the abdomen. The problem, Heppner wrote, was the tubes were prone to blocking, particularly in children. Around 50 percent of shunts in children fail in the first two years. Worse, the symptoms of a blocked tube – headaches, nausea, tiredness and irritability – could just as easily be caused by something far less dangerous.
Adults with hydrocephalus, and parents of children with the condition, are constantly on a knife-edge looking for symptoms and then having to decide whether to rush to hospital or go to bed with paracetamol. Could Malpas design a non-blocking tube? Malpas looked into it and had some bad news and some good news for the neurosurgeon. “I knew fixing the problem of the shunts failing would be incredibly challenging – hundreds and hundreds of people had tried that without success.”
But what if you could come up with a sensor which could measure brain pressure – in a patient's home – so if someone with hydrocephalus got a headache they knew whether their shunt was failing or not?
“There began the journey,” Malpas says. “I thought ‘maybe I can get a little grant and a student to explore this’. And that looked promising, so we came up with early concept ideas, and then in 2017 we got an MBIE [Ministry of Business, Innovation and Employment] Endeavour grant for $12 million and the whole team came together.”
Wireless power was a part of what was needed to build a brain sensor. But it wasn’t the only part. The device needed to be implantable. It needed to be tiny (the final sensor is about the size of a stubby matchstick). And it needed complex miniaturised electronic components to be encased in a tube made of an inert material, so the circuitry wouldn’t harm the patient’s brain or cause the sensor to be rejected – and the brain tissue wouldn’t damage the electronics.
In his own Auckland Bioengineering Institute he found Associate Professor David Budgett. Born in New Zealand, Budgett had done a PhD in biomedical engineering at Imperial College in London based on measuring and interpreting cardiac electrical signals. He was then enticed back to New Zealand by Distinguished Professor Sir Peter Hunter and the world-leading research being done around the heart at the Auckland Bioengineering Institute.
“I was very fortunate that David was back at the University. He was an electronic engineer, and he was working on instrumentation for mapping of the heart, but I dragged him into our area to work on our sensor.“
The collaboration turned out well; Budgett was part of the team using wireless power to enable implantable physiological monitoring devices. When a company, Telemetry Research, was created, Budgett became chief technology officer.
Budgett was the perfect person to develop the sensor, Malpas says, but making it small enough to implant into someone’s brain needed other skills. And in the School of Chemical Sciences he found Dr Bryon Wright.
Wright had begun his biomedical engineering career in his native US, but after moving to Auckland became fascinated by miniaturisation, and in 2012 founded the Auckland Microfab a University of Auckland research facility helping academic and industrial researchers make really small stuff.
“I met Bryon sailing,” Malpas remembers. “He was commodore of Richmond Yacht Club in Westhaven, and I was doing a trip to Tonga and was looking for crew. We had seven days at sea to talk. He was working in microfabrication; though it wasn’t in medicine, he had the right skillset.”
Wright was keen; he liked the idea of microfabrication being used to make a difference to patients. When Kitea Health was spun out of the Auckland Bioengineering Institute in 2022, Wright was co-founder and chief technology officer.
To get successful projects off the ground you need a bit of luck and serendipity. But you also need to have people on the ground with the skills and the science.
Simon Malpas says, “You need more things in the pot, more atoms bouncing around in the coffee cup, and then you get these ideas. If Bryon had not come to New Zealand, if David had not come back…”

‘Crazy ideas is science happening’
Grant Covic sees research as an ecosystem built on the foundation of blue sky exploration. Funding needs to go into science that can be commercialised in the near future and science that might be years away from a practical application. Decades working on wireless power has taught him that both university-based and industry-led research and funding are critical.
Professor Grant Covic, Faculty of Engineering and Design, Waipapa Taumata Rau, University of Auckland.
Professor Grant Covic, Faculty of Engineering and Design, Waipapa Taumata Rau, University of Auckland.
“Our early work was supported by industry, through UniServices. Then after we scaled up we received our first science funding. Over the last ten years it has been MBIE [Ministry of Business, Innovation and Employment] Endeavour funding that has enabled us to expand into a number of different fields and create new solutions that industry didn’t even know they needed.”
The advantage of University-based research is being able “to look into the future and solve problems five, ten, twenty years in the future, but at the same time solve problems that are needed tomorrow,” Covic says. “The solutions we created ended up being relevant for a number of different applications and different industries including, in the end, biomedical.”
Funding basic science also means that when companies call on researchers to solve a problem, the creative people and the underpinning knowledge is available. Covic says.“ We acknowledge we have to solve industrial and commercial problems, and we are going to do that. But if we just relied on that without the fundamental knowledge we would never have done what we did.”
Covic remembers how John Boys encouraged colleagues and students to bounce ideas around. “John Boys always said crazy ideas are great – that we shouldn’t throw them out today because they will be useful tomorrow. “Crazy ideas is science happening.”
“Innovation needs the whole gamut of funding and support."
Dr Diana Siew is a medtech innovation sector specialist heading up development of Medtech-iQ Aotearoa, a national medical devices and digital health innovation hub hosted by the University of Auckland and the Auckland Bioengineering Institute.
Siew says a vibrant technology commercialisation ecosystem needs a joined-up approach – from blue skies fundamental science at one end, to support for startup companies to take their ideas to the next level. The “valley of death” for New Zealand medtech is translating science into the commercial world, she says.
“You need the whole gamut in terms of funding and support,” she says. “Everything from MBIE Smart Ideas and the Health Research Council supporting foundation science, through early-stage translation and commercialisation with programmes like Te Tītoki Mataora and Return on Science, to company growth support like the HealthTech Activator.
“We have a good basic structure in New Zealand but all three of these areas are really important and we need to consolidate and keep building.”